There has been incredible progress in the field of cancer therapy and immunotherapy in the last decade. From the advent of Nobel Prize-winning immune checkpoint inhibitors to chimeric antigen receptor T-cells (CAR-Ts) that literally sound like the stuff sci-fi movies are made of.
In certain hematological malignancies, or blood cancers, we have learned to harness the power of the immune system to fight and eradicate cancer cells. Just a decade ago, patients diagnosed with aggressive hematological malignancies such as diffuse large B-cell lymphoma (DLBCL) or acute lymphoblastic lymphoma (ALL), whose cancer did not respond to chemotherapy, essentially had no meaningful chance at survival.
Since approximately eight years ago, we have been able to treat these patients using their own immune systems.
So what exactly are CAR-Ts?
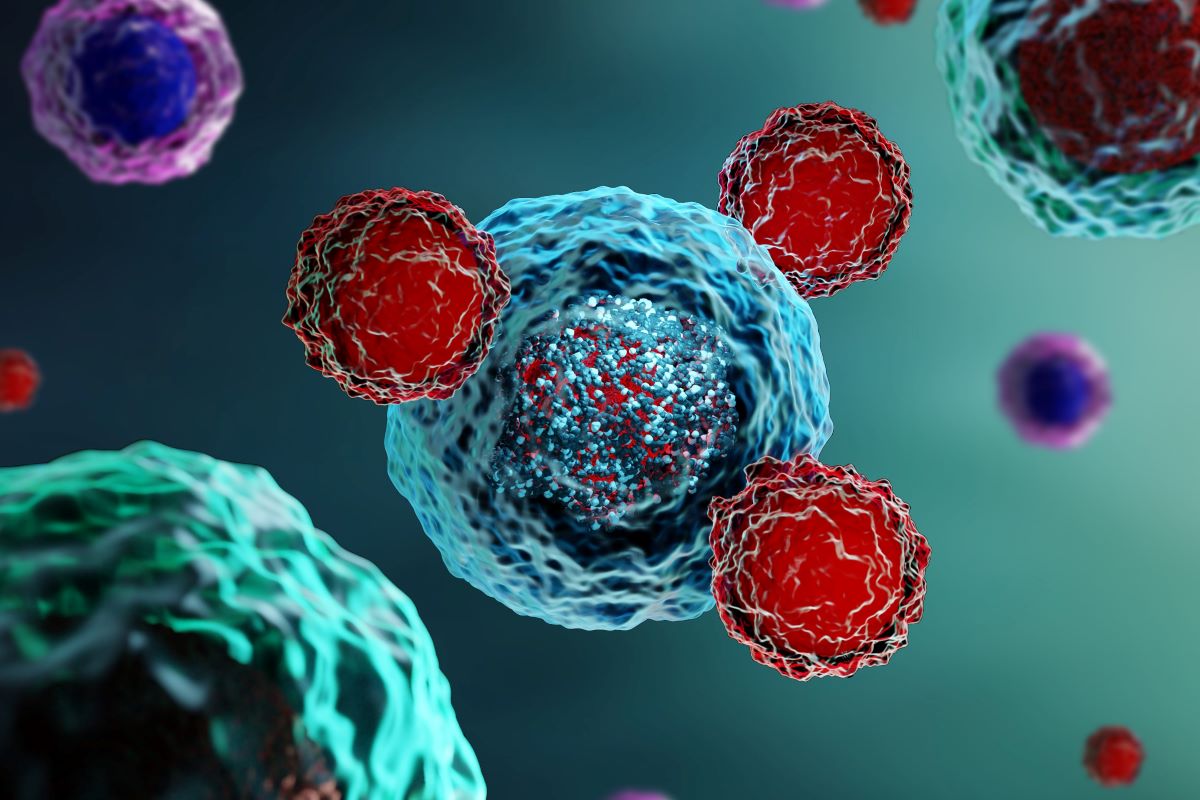
Our immune system is complex and made up of different cell types with different functions and “training” levels. T-cells are a natural part of our immune system that help eradicate infections. They also orchestrate other parts of the immune system. T-cells are taken from a patient’s body using a process called apheresis. They are then genetically modified to make them think the cancer cells are an infection that must be eradicated.
Those modified cells are now called CAR-Ts. They must be infused back into the patient’s body at specialized centers where an expert team is able to recognize and treat the unique side effects that come with these therapies.
These therapies have provided new hope for a portion of patients who had none before. As of today, there are seven FDA-approved CAR-Ts to treat seven different types of hematological malignancies. They all differ slightly from each other, and their proper application has a unique impact on a patient’s journey.
Tumor-infiltrating lymphocytes, or TILs for short, are another novel and promising form of immunotherapy. TILs are currently only approved for melanoma but are under investigation for a variety of different cancers.
TILs are also T-cells that have infiltrated, or penetrated, the cancer mass but seem to be overpowered. The whole cancer mass is surgically removed, and the TILs are extracted and expanded to increase their number and cancer-fighting abilities. They are then reinfused into the patient’s body after some chemotherapy.
TILs also represent a very promising approach to treat cancers for which standard therapies have not worked. It requires a tight-knit team to coordinate the surgery with the processing of the cells and the reinfusion, as well as to care for the patient while all this is happening.
Despite these advances, there are still many more patients in need of further therapies. These available therapies can also be improved upon. However, the future is bright, with many different types of cellular and immunotherapies being investigated in a wide variety of clinical trials to make them safer, better and more accessible.
The Blood and Marrow Transplant Group of Georgia has been a national leader in the delivery of these complex treatments, as well as in offering cutting-edge clinical trials for those who would need them.
Learn more about CAR T-cell treatment at Northside Hospital.

