Gastroenterological complaints account for a significant number of visits to primary care offices and contribute substantially to morbidity in the population. Some conditions are more easily diagnosed than others, and not infrequently the issue evades a definitive diagnosis.
Irritable bowel syndrome (IBS) is frequently the diagnosis once other conditions have been ruled out. However, it is merely a diagnosis of exclusion and not one of etiology or pathophysiology.
According to a 2020 meta-analysis of 25 case-control studies involving 3,192 IBS subjects and 3,320 controls, the prevalence of small intestinal bacterial overgrowth (SIBO) in IBS was 31 percent when compared with controls. This offers little benefit in terms of therapeutic or curative options.
SIBO is characterized by excessive bacterial proliferation in the small intestine, exceeding the typical concentrations found in this region of the gastrointestinal tract. Under normal circumstances, the small intestine maintains a relatively low bacterial population — rarely exceeding 1,000 organisms per milliliter —due to protective mechanisms such as gastric acid secretion and peristalsis. When these defenses are compromised, bacterial overgrowth can occur, leading to various gastrointestinal symptoms and potential malabsorption.
Etiology and risk factors
Several factors can disrupt the balance of the small intestine’s microbiota and lead to SIBO. These include:
- Motility disorders: Impaired intestinal motility can result in stagnation of intestinal contents, providing an environment conducive to bacterial overgrowth. Conditions such as scleroderma and diabetic neuropathy are associated with motility issues.
- Anatomical abnormalities: Structural changes such as small intestinal diverticula, strictures or surgical alterations (for example, blind loops or resection of the ileocecal valve) can create areas where bacteria can accumulate and proliferate.
- Gastric acid suppression: The use of proton pump inhibitors or conditions leading to achlorhydria reduces gastric acidity, diminishing its bactericidal effect and allowing more bacteria to survive and colonize the small intestine.
- Immune system disorders: Immunodeficiency syndromes can impair the body’s ability to regulate bacterial populations in the gut, facilitating overgrowth.
- Pancreatic insufficiency: Inadequate production of pancreatic enzymes can lead to improper digestion, providing substrates for bacterial fermentation and growth.
Clinical manifestations
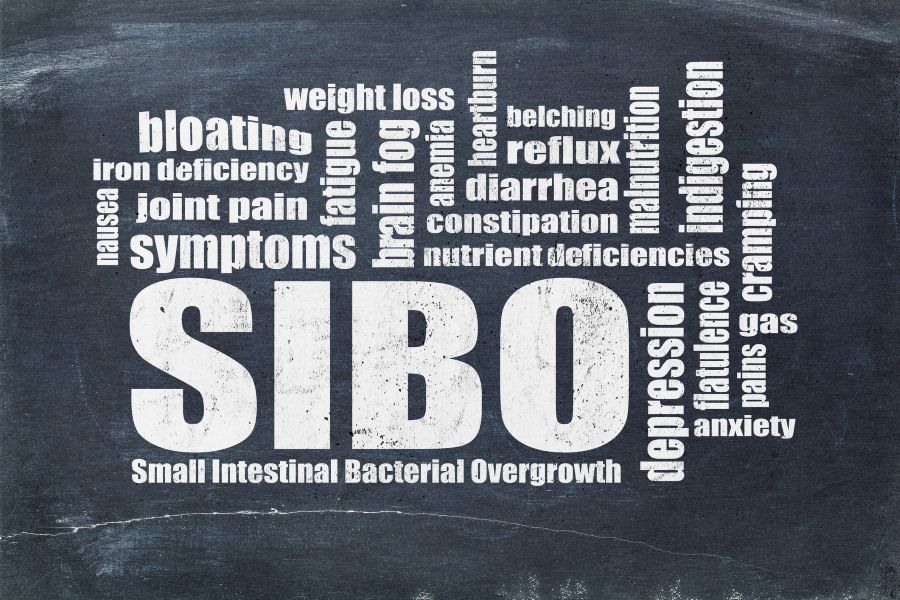
Symptoms of SIBO are often nonspecific and can overlap with other gastrointestinal disorders, making diagnosis challenging. Common manifestations include:
- Gastrointestinal symptoms: Patients may experience bloating, abdominal pain or discomfort, diarrhea and, in some cases, constipation. Steatorrhea, characterized by fatty stools, can occur in more severe cases because of fat malabsorption.
- Nutritional deficiencies: Chronic SIBO can lead to malabsorption of nutrients, resulting in deficiencies such as vitamin B12 deficiency, iron deficiency anemia and fat-soluble vitamin deficiencies. The overgrown bacteria consume nutrients and interfere with absorption.
- Systemic symptoms: Some individuals may experience fatigue, weakness and weight loss due to malabsorption and chronic inflammation.
Understanding these symptoms can give clinicians an index of suspicion to consider SIBO in the differential diagnosis. If suspicion is high enough or if other diagnoses have been ruled out, testing should be explored.
Diagnosing SIBO requires a combination of clinical evaluation and diagnostic testing:
- Breath tests: Hydrogen and methane breath tests are commonly used noninvasive methods. After ingestion of a carbohydrate substrate such as lactulose or glucose, measurements of hydrogen and methane gases are taken. Elevated levels suggest bacterial fermentation, indicative of SIBO. However, these tests carry limitations, including false positives and false negatives.
- Jejunal aspirate and culture: Considered the gold standard, this invasive procedure involves obtaining a fluid sample from the small intestine for bacterial culture. A bacterial count exceeding 10⁵ organisms per milliliter is diagnostic for SIBO.
- Laboratory tests: Blood tests may reveal nutritional deficiencies, such as low vitamin B12 or elevated folate levels, supporting the diagnosis.
When the appropriate tests are combined with clinical judgment, clinicians can move forward with a comprehensive treatment regimen.
Treatment
Management of SIBO focuses on addressing the underlying cause, reducing bacterial overgrowth and correcting nutritional deficiencies:
- Antibiotic therapy: Broad-spectrum antibiotics such as rifaximin are commonly prescribed to reduce bacterial populations in the small intestine. Treatment duration varies but typically lasts 10 to 14 days.
- Dietary modifications: Dietary interventions such as low-FODMAP diets aim to reduce fermentable substrates that bacteria utilize, thereby decreasing symptoms.
- Probiotics: Probiotics aim to restore a healthy balance of gut microbiota. Certain strains, including Lactobacillus and Bifidobacterium, have shown promise in reducing bacterial overgrowth and alleviating symptoms. Responses vary, however, and some individuals may experience worsening symptoms. It is essential to consult a health care provider before starting supplementation.
- Addressing underlying conditions: Identifying and managing predisposing factors, such as improving gut motility or discontinuing unnecessary proton pump inhibitors, is crucial to preventing recurrence.
Conclusion
SIBO is a complex condition resulting from an imbalance in the small intestine’s bacterial population, leading to a range of gastrointestinal and systemic symptoms. Understanding its risk factors, clinical manifestations and diagnostic challenges is essential for effective management. Awareness of the condition and including it in the differential diagnosis may help clinicians arrive at a definitive diagnosis sooner, ultimately providing more timely relief for those affected.
LEARN MORE ABOUT PRIMARY CARE AT NORTHSIDE.
This article appeared in the Summer 2025 issue of Scripts.

